Oral cancer
Oral cancer, also known as mouth cancer, is cancer of the lining of the lips, mouth, or upper throat.[5] In the mouth, it most commonly starts as a painless white patch, that thickens, develops red patches, an ulcer, and continues to grow. When on the lips, it commonly looks like a persistent crusting ulcer that does not heal, and slowly grows.[6] Other symptoms may include difficult or painful swallowing, new lumps or bumps in the neck, a swelling in the mouth, or a feeling of numbness in the mouth or lips.[7]
Risk factors include tobacco and alcohol use.[8][9] With both tobacco and drinking alcohol the risk of oral cancer is 15 times greater.[10] Other risk factors include HPV infection,[11] chewing paan,[12] and sun exposure on the lower lip.[13] Oral cancer is a subgroup of head and neck cancers.[5] Diagnosis is made by biopsy of the concerning area, followed by investigation with CT scan, MRI, PET, and examination to determine if it has spread to distant parts of the body.
Oral cancer can be prevented by avoiding tobacco products, limiting alcohol use, sun protection on the lower lip, HPV vaccination, and avoidance of paan. Treatments used for oral cancer can include a combination of surgery (to remove the tumor and regional lymph nodes), radiation therapy, chemotherapy or targeted therapy. The types of treatments will depend on the size, locations, and spread of the cancer taken into consideration with the general health of the person.[6]
In 2018, oral cancer occurred globally in about 355,000 people, and resulted in 177,000 deaths.[4] Between 1999 and 2015 in the United States rate of oral cancer increased 6% (from 10.9 to 11.6 per 100,000). Even though smoking cessation campaigns have decreased the rate of tobacco induced tumors, the rate of HPV related cancers has offset the gains. Deaths from oral cancer during this time deceased 7% (from 2.7 to 2.5 per 100,000).[14] Oral cancer has an overall 5 year survival rate of 63%.[15]This varies depending on how advanced it is when diagnosed. If treated early in the disease, oral cancer has an 84% 5-year survival rate, compared to 65% if it has spread to the lymph nodes in the neck, and 39% if it has spread to distant parts of the body.[16] Survival rates also are dependent on the location of the disease in the mout
Signs and symptoms
The signs and symptoms of oral cancer depend on the location of the tumor but are generally thin, irregular, white patches in the mouth. They can also be a mix of red and white patches (mixed red and white patches are much more likely to be cancerous when biopsied). The classic warning sign is a persistent rough patch with ulceration, and a raised border that is minimally painful. On the lip, the ulcer is more commonly crusting and dry, and in the pharynx it is more commonly a mass. It can also be associated with a white patch, loose teeth, bleeding gums, persistent ear ache, a feeling of numbness in the lip and chin, or swelling.[18]
When the cancer extends to the throat, there can also be difficulty swallowing, painful swallowing, and an altered voice.[19] Typically, the lesions have very little pain until they become larger and then are associated with a burning sensation.[20] As the lesion spreads to the lymph nodes of the neck, a painless, hard mass will develop. If it spreads elsewhere in the body, general aches can develop, most often due to bone metastasis.[20]
Causes
Oral squamous cell carcinoma is a disease of environmental factors, the greatest of which is tobacco. Like all environmental factors, the rate at which cancer will develop is dependent on the dose, frequency and method of application of the carcinogen (the substance that is causing the cancer).[21] Aside from cigarette smoking, other carcinogens for oral cancer include alcohol, viruses (particularly HPV 16 and 18), radiation, and UV light.[6]
Tobacco
Tobacco is the greatest single cause of oral and pharyngeal cancer. It is a known multi-organ carcinogen, that has a synergistic interactionwith alcohol to cause cancers of the mouth and pharynx by directly damaging cellular DNA.[21] Tobacco is estimated to increase the risk of oral cancer by 3.4[21]-6.8[8] and is responsible for approximately 40% of all oral cancers.[22]
Alcohol
Some studies in Australia, Brazil and Germany pointed to alcohol-containing mouthwashes as also being potential causes. The claim was that constant exposure to these alcohol-containing rinses, even in the absence of smoking and drinking, leads to significant increases in the development of oral cancer. However, studies conducted in 1985,[23] 1995,[24]and 2003[25] summarize that alcohol-containing mouth rinses are not associated with oral cancer. In a March 2009 brief, the American Dental Association said "the available evidence does not support a connection between oral cancer and alcohol-containing mouthrinse".[26] A 2008 study suggests that acetaldehyde (a breakdown product of alcohol) is implicated in oral cancer,[27][28] but this study specifically focused on abusers of alcohol and made no reference to mouthwash. Any connection between oral cancer and mouthwash is tenuous without further investigation.
Human papillomavirus
Infection with human papillomavirus (HPV), particularly type 16 (there are over 180 types), is a known risk factor and independent causative factor for oral cancer.[29] A fast-growing segment of those diagnosed does not present with the historic stereotypical demographics. Historically that has been people over 50, blacks over whites 2 to 1, males over females 3 to 1, and 75% of the time people who have used tobacco products or are heavy users of alcohol. This new and rapidly growing sub population between 30 and 50 years old,[30] is predominantly nonsmoking, white, and males slightly outnumber females. Recent research from multiple peer-reviewed journal articles indicates that HPV16 is the primary risk factor in this new population of oral cancer victims. HPV16 (along with HPV18) is the same virus responsible for the vast majority of all cervical cancers and is the most common sexually transmitted infection in the US. Oral cancer in this group tends to favor the tonsil and tonsillar pillars, base of the tongue, and the oropharynx. Recent data suggest that individuals that come to the disease from this particular cause have a significant survival advantage,[31] as the disease responds better to radiation treatments than tobacco caused disease.
Betel nut
Chewing betel, paan and Areca is known to be a strong risk factor for developing oral cancer even in the absence of tobacco. It increases the rate of oral cancer 2.1 times, through a variety of genetic and related effects through local irritation of the mucous membrane cells, particularly from the areca nut and slaked lime.[21] In India where such practices are common, oral cancer represents up to 40% of all cancers, compared to just 4% in the UK.
Stem cell transplantation
People after hematopoietic stem cell transplantation (HSCT) are at a higher risk for oral squamous cell carcinoma. Post-HSCT oral cancer may have more aggressive behavior with poorer prognosis, when compared to oral cancer in people not treated with HSCT.[32] This effect is supposed to be owing to the continuous lifelong immune suppression and chronic oral graft-versus-host disease.[32]
Premalignant lesions
A premalignant (or precancerous) lesion is defined as "a benign, morphologically altered tissue that has a greater than normal risk of malignant transformation." There are several different types of premalignant lesion that occur in the mouth. Some oral cancers begin as white patches (leukoplakia), red patches (erythroplakia) or mixed red and white patches (erythroleukoplakia or "speckled leukoplakia"). Other common premalignant lesions include oral submucous fibrosis and actinic cheilitis.[33] In the Indian subcontinent oral submucous fibrosis is very common due to betel nut chewing. This condition is characterized by limited opening of mouth and burning sensation on eating of spicy food. This is a progressive lesion in which the opening of the mouth becomes progressively limited, and later on even normal eating becomes difficult. It occurs almost exclusively in India and Indian communities living abroad.
Pathophysiology
Oral squamous cell carcinoma is the end product of an unregulated proliferation of mucous basal cells. A single precursor cell is transformed into a clone consisting of many daughter cells with an accumulation of altered genes called oncogenes. What characterizes a malignant tumor over a benign one is its ability to metastasize. This ability is independent of the size or grade of the tumor (often seemingly slow growing cancers like the adenoid cystic carcinoma can metastasis widely). It is not just rapid growth that characterizes a cancer, but their ability to secrete enzymes, angiogeneic factors, invasion factors, growth factors and many other factors that allow it to spread.[6]
Diagnosis
Diagnosis of oral cancer is completed for (1) initial diagnosis, (2) staging, and (3) treatment planning. A complete history, and clinical examination is first completed, then a wedge of tissue is cut from the suspicious lesion for tissue diagnosis. This might be done with scalpel biopsy, punch biopsy, fine or core needle biopsy. In this procedure, the surgeon cuts all, or a piece of the tissue, to have it examined under a microscope by a pathologist.[34] Brush biopsies are not considered accurate for the diagnosis of oral cancer.[35]
With the first biopsy, the pathologist will provide a tissue diagnosis (e.g. squamous cell carcinoma), and classify the cell structure. They may add additional information that can be used in staging, and treatment planning, such as the mitotic rate, the depth of invasion, and the HPVstatus of the tissue.
After the tissue is confirmed cancerous, other tests will be completed to:
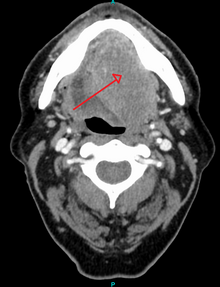
- better assess the size of the lesion (CT scan, MRI or PET scan with 18F-fluorodeoxyglucose (FDG)),[34](pp143)
- look for other cancers in the upper aerodigestive tract (which may include endoscopy of the nasal cavity/pharynx, larynx, bronchus, and esophagus called panendoscopy or quadoscopy),
- spread to the lymph nodes (CT scan) or
- spread to other parts of the body (chest x-ray, nuclear medicine).
Other, more invasive tests, may also be completed such as fine needle aspiration, biopsy of lymph nodes, and sentinel node biopsy. When the cancer has spread to lymph nodes, their exact location, size, and spread beyond the capsule (of the lymph nodes) needs to be determined, as each can have a significant impact on treatment and prognosis. Small differences in the pattern of lymph node spread, can have a significant impact on treatment and prognosis. Panendoscopy may be recommended, because the tissues of the entire upper aerodigestive tract are generally affected by the same carcinogens, so other primary cancers are a common occurrence.
From these collective findings, taken in consideration with the health and desires of the person, the cancer team develops a plan for treatment. Since most oral cancers require surgical removal, a second set of histopathologic tests will be completed on any tumor removed to determine the prognosis, need for additional surgery, chemotherapy, radiation, immunotherapy, or other interventions.
Screening
The US Preventive Services Task Force (USPSTF) in 2013 stated evidence was insufficient to determine the balance of benefits and harms of screening for oral cancer in adults without symptoms by primary care providers.[38] The American Academy of Family Physicians comes to similar conclusions while the American Cancer Society recommends that adults over 20 years who have periodic health examinations should have the oral cavity examined for cancer.[38] The American Dental Association recommends that providers remain alert for signs of cancer during routine examinations.[38]
There are a variety of screening devices, however, there is no evidence that routine use of these devices in general dental practice is helpful.[39] However, there are compelling reasons to be concerned about the risk of harm this device may cause if routinely used in general practice. Such harms include false positives, unnecessary surgical biopsies and a financial burden.
Classification
Oral cancer is a subgroup of head and neck cancers which includes those of the oropharynx, larynx, nasal cavity and paranasal sinuses, salivary glands, and thyroid gland. Oral melanoma, while part of head and neck cancers is considered separately.[5] Other cancers can occur in the mouth (such as bone cancer, lymphoma, or metastatic cancers from distant sites) but are also considered separately from oral cancers.[5]
Staging
Oral cancer staging is an assessment of the degree of spread of the cancer from its original source.[40] It is one of the factors affecting both the prognosis and the potential treatment of oral cancer.[40]
The evaluation of squamous cell carcinoma of the mouth and pharynx staging uses the TNM classification (tumor, node, metastasis). This is based on the size of the primary tumor, lymph node involvement, and distant metastasis